The Heart of a Warrior: Lauren’s Unbreakable Spirit
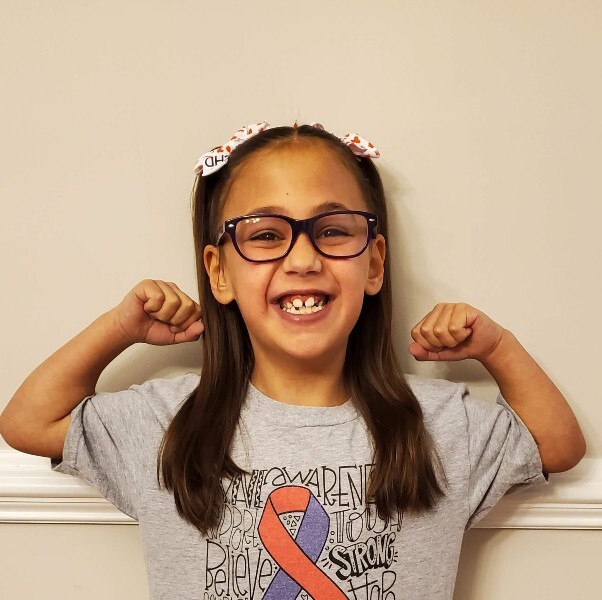
Lauren is a bright and energetic 10-year-old with a smile that lights up a room. She loves riding her bike, singing and dancing. She’s a natural on stage, thriving in the spotlight. Her bubbly personality and love of connecting with others earned her the nickname “social butterfly” from her parents—fitting since the butterfly is the symbol of Turner syndrome, one of the rare conditions she’s lived with since birth.
Behind Lauren’s vibrant personality is a long and complicated health journey. Doctors diagnosed her in utero with a high-risk combination of hypoplastic left heart syndrome (HLHS)—when the left side of the heart is underdeveloped—and Turner syndrome, a genetic disorder. “I just remember thinking, ‘How are we going to get through this?’” recalls Cara, her mom.
Children’s National Hospital became their second home. “They gave us a tour of the Cardiac Intensive Care Unit before Lauren was born,” Cara says. “It was overwhelming, but I’m thankful we got to meet the people who would care for her. It helped us process what was coming.”
At 36 weeks, Cara’s placenta shut down, and Lauren’s heart rate dropped, leading to an emergency C-section. Weighing just 4 pounds, 9 ounces, Lauren needed surgery at 6 days old. Children’s National surgeons used the smallest shunt possible—still even too large for her tiny heart. “The team was amazing,” Cara says. “They kept us updated every step of the way. I remember sitting in that hospital room, just praying that she’d be okay.”
After ten weeks in the hospital, Lauren went home with a feeding tube. At 4 months, she had a Glenn procedure, and at age 2, it was time for her Fontan surgery—both lifesaving interventions often needed by HLHS patients. Once home, Lauren began to thrive. “That’s when we could finally start living a little,” Cara says. Lauren soon started preschool.
For years, things were stable. But when she turned 9, Lauren’s cardiologist, Tom Loke, noticed her oxygen levels were off. A heart valve was leaking, and the tube created to connect parts of her heart during the Fontan procedure had become too small as she grew. “Dr. Loke explained that it wasn’t a matter of if, but when, she’d need another surgery,” Cara says.
Lauren then had her most complex surgery, led by Yves d’Udekem. Using advanced 4D Flow MRI scans, doctors could see exactly how blood was flowing through Lauren’s heart and repair her valve. They also made the tube bigger, which new research by Dr. d’Udekem shows can boost exercise capacity and ease strain on the liver long-term. Children's National is one of the only U.S. centers offering this life-changing procedure.
The results were immediate. Lauren’s oxygen levels improved, and she felt happier and had more energy. “It was a power boost—like a video game,” Cara says.
Six months later, Lauren is still thriving. At her last checkup, Dr. Loke was thrilled with how well her heart was functioning. “He said her heart looked better than it ever has,” Cara says.
The family’s anxiety about doctor’s appointments has eased, thanks to emotional support from Children’s National psychologists. “They helped me change how I approached situations so I could better support Lauren,” Cara says. “Now, after years of medical trauma, Lauren is fine at the doctor’s office. She understands what’s happening.” Visits from therapy dogs Slipper and Wilma, part of the hospital’s Animal Visitation and Therapy Program, have also helped Lauren through tough moments in the hospital.
“Children’s National has always treated us like partners in Lauren’s care,” Cara says. “They’d ask us how we felt about things and what we thought would help Lauren the most. That meant so much to us.”
Cara often reflects on how far they’ve come. “Lauren is a true heart warrior,” she says. “There were so many dark days when I wondered if we’d get to this point. But thanks to Children’s National, and Lauren’s incredible resilience, she’s dancing, laughing and dreaming about the future. She’s getting back to being a kid.”
Behind Lauren’s vibrant personality is a long and complicated health journey. Doctors diagnosed her in utero with a high-risk combination of hypoplastic left heart syndrome (HLHS)—when the left side of the heart is underdeveloped—and Turner syndrome, a genetic disorder. “I just remember thinking, ‘How are we going to get through this?’” recalls Cara, her mom.
Children’s National Hospital became their second home. “They gave us a tour of the Cardiac Intensive Care Unit before Lauren was born,” Cara says. “It was overwhelming, but I’m thankful we got to meet the people who would care for her. It helped us process what was coming.”
At 36 weeks, Cara’s placenta shut down, and Lauren’s heart rate dropped, leading to an emergency C-section. Weighing just 4 pounds, 9 ounces, Lauren needed surgery at 6 days old. Children’s National surgeons used the smallest shunt possible—still even too large for her tiny heart. “The team was amazing,” Cara says. “They kept us updated every step of the way. I remember sitting in that hospital room, just praying that she’d be okay.”
After ten weeks in the hospital, Lauren went home with a feeding tube. At 4 months, she had a Glenn procedure, and at age 2, it was time for her Fontan surgery—both lifesaving interventions often needed by HLHS patients. Once home, Lauren began to thrive. “That’s when we could finally start living a little,” Cara says. Lauren soon started preschool.
For years, things were stable. But when she turned 9, Lauren’s cardiologist, Tom Loke, noticed her oxygen levels were off. A heart valve was leaking, and the tube created to connect parts of her heart during the Fontan procedure had become too small as she grew. “Dr. Loke explained that it wasn’t a matter of if, but when, she’d need another surgery,” Cara says.
Lauren then had her most complex surgery, led by Yves d’Udekem. Using advanced 4D Flow MRI scans, doctors could see exactly how blood was flowing through Lauren’s heart and repair her valve. They also made the tube bigger, which new research by Dr. d’Udekem shows can boost exercise capacity and ease strain on the liver long-term. Children's National is one of the only U.S. centers offering this life-changing procedure.
The results were immediate. Lauren’s oxygen levels improved, and she felt happier and had more energy. “It was a power boost—like a video game,” Cara says.
Six months later, Lauren is still thriving. At her last checkup, Dr. Loke was thrilled with how well her heart was functioning. “He said her heart looked better than it ever has,” Cara says.
The family’s anxiety about doctor’s appointments has eased, thanks to emotional support from Children’s National psychologists. “They helped me change how I approached situations so I could better support Lauren,” Cara says. “Now, after years of medical trauma, Lauren is fine at the doctor’s office. She understands what’s happening.” Visits from therapy dogs Slipper and Wilma, part of the hospital’s Animal Visitation and Therapy Program, have also helped Lauren through tough moments in the hospital.
“Children’s National has always treated us like partners in Lauren’s care,” Cara says. “They’d ask us how we felt about things and what we thought would help Lauren the most. That meant so much to us.”
Cara often reflects on how far they’ve come. “Lauren is a true heart warrior,” she says. “There were so many dark days when I wondered if we’d get to this point. But thanks to Children’s National, and Lauren’s incredible resilience, she’s dancing, laughing and dreaming about the future. She’s getting back to being a kid.”


Be the Reason a Child Smiles
Every day at Children’s National Hospital, lives are changed through compassionate care and groundbreaking discoveries. Your charitable donation helps us deliver expert treatment and hope to thousands of children and families.
Meet the patients whose stories inspire us—and see the difference your support makes.



